HEALTHCARE PROFESSIONALS
Online Resources for Healthcare Professionals
For Medical Professionals: Northern Light Home Care & Hospice - Northern Light Health
Home Care & Hospice Alliance of Maine
By: David Jones, MD, FAAFP
Medical Director Northern Light Home Care & Hospice, Medical Director Community Hospice North, Medical Director House of Comfort, Presque Isle
Hospice Care
By: David Jones, MD, FAAFP
Medical Director Northern Light Home Care & Hospice, Medical Director Community Hospice North, Medical Director House of Comfort, Presque Isle
Living Longer, Dying Slower
- Maine is the “oldest state” in the US, average age 44.8 (Utah 35.5).
- Aroostook County is the “oldest county” in Maine average, age is 48.
- The LOL in the US increased 10 years between 1960 and 2015, and now (estimated for 2022) is 79.05, increasing 0.08% a year. It is expected to increase by 6.1 years to 85.6 over the next 45 years.
- The care of the elderly with cancers and chronic illness will continue to grow
Comfort Care
- Comfort Care really equals End of Life Care and is a synonym of Palliative Care or Hospice Care.
- Care at the end of life (National Institute of Aging) involves 4 categories of care:
- Physical
- Emotional
- Spiritual
- Practical
Care at the End of Life
- Physical: Pain, Breathing, Skin, GI, Temperature, Fatigue.
- Emotional: Depression, Anxiety.
- Spiritual: Past, Present, Future. Sacrament of the Sick.
- Practical: Bucket list, Financial, Will.
Communication
- The patient needs to drive the “bus”
- What is Comfort Care? It is what the patient wants at the end of life, without aggressive intervention, developed by discussions with the patient, family, and provider.
- The provider needs to identify the goals of patient and family. Only 40% of adult Americans have a living will.
- Living Will = Advanced Directive ≠ POLST
- The patient needs to be encouraged to fill out a POLST and ideally a living will. These forms are self-explanatory, the POLST has more medical detail and the living will has more legal detail.
- The POLST is in effect when signed, the Living Will is legal when signed but not in effect until the patient is not mentally competent.
- The patient needs to be clear when the medical POA goes into effect.
End of Life Planning
- Identify the patient goals.
- Tell the patient what will happen next. Do not guess at length of life.
- Discuss testing/treatment and the actual benefits, or lack thereof, from either.
- The effect of the previous line on the speed and symptoms of the dying process.
- Evaluate the capacity and capability of the caregiver.
- Can the caregiver continue, does she/he have help?
Stop
- For any End-of-Life patient consider:
- Stopping all medications that do not give comfort and stopping anticoagulants (risk vs benefit).
- Stop needle sticks (blood draws or IM meds, and most finger sticks)
- Stop diagnostic studies (imaging) and therapies.
- Consider single dose long-acting insulin daily, allow blood sugars to run high, perform rare finger sticks.
- Comfort care does not mean stopping ALL MEDICINES.
- Providing medicines or interventions to treat the 4 categories of care at the End of Life discussed earlier i.e. weighted blanket, pool noodles, humidifier, commode, increased heat, social worker, spiritual councilor or volunteers.
Deprescribing
- Consider length to benefit
- Risk vs benefit
- Goals of treatment in Hospital and after discharge
- Involve patent, family and or POA
- Many meds can be stopped immediately, some need to be tapered
- Stop statins, appetite stimulants, platelet drugs unless stent within 1 year, stop anticoagulants, inhaled steroids, and bronchodilators
- Stop aces and arbs, stop most oral diabetic meds,
- Decrease PPIs and diuetics.
- Taper or decrease BBs and calcium channel blockers
- while monitoring pulse. Taper and stop other antihypertensives.
- Decrease memory drug in half for 1-2 weeks and then stop, if on a second, then only after the first is stopped, wean the second.
- Do not stop antidepressants or behavior meds, do not stop steroids, if patient has a foley, only then stop all bladder outlet obstruction meds.
Communication
You need to be very clear in long term care orders about transport/no transport to the hospital. Asking the patient and family to reconsider multiple times increases poor outcomes, increased grief, and increased guilt.
Notification of illness or injury is very different than asking them if they want their loved one transported to the hospital for “evaluation and care.”
Palliative Care Definition
NHPCO (National Hospice and Palliative Care Organization):
Palliative Care is patient and family centered care that optimizes quality of life by anticipating preventing and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and to facilitate patients’ autonomy, access to information and choice.
Hospice Definition
NHPCO (National Hospice and Palliative Care Organization):
Hospice care is considered to be the model of quality, compassionate care for people facing a life-limiting illness or injury and involves a team-orientated approach to expert medical care, pain management and emotional and spiritual support expressly tailored to the patients’ needs and wishes. Support is provided to the patient’s loved ones as well. At the center of Hospice and Palliative Care is the belief that each of us has the right to live pain free and with dignity, and that our families will receive the necessary support to allow us to do so.
Hospice-Palliative Care
Length and quality of life are both improved by these services. Palliative Care and Hospice Care are gradually becoming seamless as the patients’ needs move from symptom management to the end-of-life care. Stage 4 cancer LOL and quality of life have been proven to be increased by changing to or incorporating the Hospice model as opposed to aggressive pursuit of disease modifying treatments.
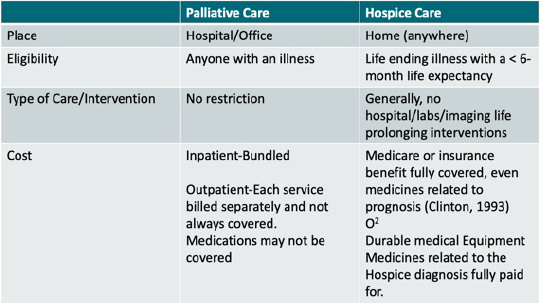
Major Differences in Palliative vs. Hospice Care
Hospice is Composed of an Interdisciplinary Team
- Administration
- Local Supervisor
- Hospice Physician
- Nurse Practitioners
- RN’s
- Social Workers
- Chaplains (spiritual councilor)
- Volunteer Coordinator (and volunteers)
- Home Health Aides
- PT/OT – massage, music, other
Hospice Offers
- Interdisciplinary team care
- Medical appliances and supplies (durable medical supplies).
- Medicines for pain and symptom management.
- Medicines related to the patient’s health-prognosis that he/she is currently taking.
- Face to face visits by a hospice nurse practitioner or the Hospice Physician – either initially or for recertification, or again, the Hospice Physician, in unusual situations.
- Bereavement services (13 months)
- Availability of the Hospice Physician 24/7 for phone consultations on pain and symptom management or diagnosis.
- Availability of a Hospice Pharmacist for consultation.
Location of Care: ANYWHERE!
- Home, nursing home, assisted living, boarding home, anyplace the patient calls home.
Types of Care
- Routine – Outpatient Hospice Care
- Continuous – Short term minimum of 8 hours RN/SW care in the Home, Medicare now wants this before a GIP admission. (rare).
- Respite – 5 days out of current living situation- occurs in a Hospice House or NH.
- GIP – Pain and Symptom management that is usually in a hospital or hospice house that represents a crisis and can’t be occur in another setting.
At the House of Comfort, when patients no longer qualify for GIP, they can return to their previous living situation, self-pay to stay at the House of Comfort (limited) or be placed in LTC, depending on the situation.
- Hospice encourages continued involvement in the hospice care (and follow-up visits) of a patient by their primary care provider or the oncologist if he/she is interested.
- I am generally a consultant, although I assume the provider role if the hospice patient does not have an attending physician and assume medical management if requested or expected to.
- Hospice may cover palliative or other interventions.
- Medicare will occasionally cover acute interventions (fracture/fall/burns/diseases not related to the Hospice diagnosis) depending on the cause. Patients need to understand that if they return to the hospital and their hospice plan of care does not include an acute intervention (ie repair of a fractured hip), their ED visit may be covered but further intervention probably will not be, and they would have a choice to revoke for treatment or return home.
Hospice Events
- Informing visit – RN, SW, MD (Hospice Physician)- necessary before admission
- Admission
- Routine/Respite/GIP/Continuous Care
- Revocation
- Discharge for moving/transition to a competing local house, or admission away hospice, or admission to facility that does not accept hospice.
- Discharge for cause.
- “Graduation” if patient’s health status improves (no longer has a life expectancy <6 months).
Hospice Does Not
Hospice does not generally pay for:
- Lab (except occasionally PT/INRs or U/As without culture or other labs in certain circumstances)
- Imaging (except in certain circumstances)
- Specialty care with interventions, OP provider visits are billed to Medicare or other insurances
- Life prolonging interventions
If the patient still wants tests, treatments, or ED visits, consider skilled palliative care in the home with transition to hospice.
Hospice Facts
The National Hospice and Palliative Care Organization (NHPCO):
“Facts and Figures 2021 edition (revision 8/2021)
This publication uses data from patients who received the hospice benefit from Medicare in 2019.
- 1.61 million Medicare beneficiaries were enrolled >1 day of hospice in 2018.
- 51.6% of all Medicare decedents had 1 day of hospice or more of Hospice care.
State ranking for descendent hospice enrollment (the %) of Medicare patients who died in the state who were in hospice in 2018).
- Utah: 60.8% (1st)
- Alaska: 22.8% (51st)
- Maine: 51.4% (16th out of 52)
- Enrollment. 56.1% female, 46.1% male.
- Length of stay is skewed to short stays:
- 10% of hospice patients were enrolled for 2 days or less
- 25% of hospice patients were enrolled for 5 days or less
- 50% of hospice patients were enrolled for 18 days or less
- 75% of hospice patients were enrolled for 85 days or less
- 90% of hospice patients were enrolled for 266 days or less.
Average lifetime length of stay 89.6 days
Days of care by diagnosis
- Alzheimer’s disease/Dementia/Parkinson’s disease: Average length of stay 126 days.
- Chronic kidney disease: Average length of stay 35.6.
- All other cancers and medical diseases fall between these 2 length of stays.
Hospice cost to Medicare
- 20.9 billion dollars in 2019.
- 15.9 billion dollars in 2015.
Medicare Hospice Spending (2019):
- Cost for routine hospice care: 93.8% of Medicare hospice budget, 98.3% of actual care
- Cost for GIP hospice care: 4.9% of Medicare hospice budget, 1.2% of actual care.
- Cost for respite hospice care: 0.3 OF Medicare hospice budget, 3% of actual care.
- Cost for continuous hospice care: 0.9% of the Medicare hospice budget, 0.2 % of actual care.
- Medicare certified Hospices in 2018 – 4639, a 13.4 increase from 2014, and 4840 Medicare certified hospices in 2019, an 18.3 increase from 2014.
- Average daily census for US Hospice programs: 69.9 mean 31.8 (2018).
- 63% of Hospice had <50 patients enrolled, 1% > 500 patients (2018).
- For profit 71% (2019).
- Not for profit 26% (2019).
- Government facilities 3% (2019).
Qualifications for Hospice
Who Qualifies for Hospice
- The patient needs a Hospice benefit qualifying diagnosis, with documentation of decline prior to admission, especially for medical diagnosis.
- The referring physician has to sign a CTI (Certificate of Terminal Illness) stating the patient has terminal illness with a 6 month or less life expectancy. The Hospice Physician also has to sign a CTI.
- The Patient or POA has to sign a statement accepting the hospice benefit.
- Hospice is a Medicare Part A benefit.
- The patient usually needs a primary caregiver (family, friend, paid caregiver) or a willingness to make plans for future living arrangements, with family, friend as a resident in a long-term care facility.
- Medicare is specific in the criteria needed for each disease category to qualify for the hospice benefit.
- Other insurances generally follow Medicare’s rules.
- The primary diagnosis needs a life expectancy equal to or less than 6 months, and comorbidities can support a primary diagnosis that may not fully qualify for the Hospice benefit on its own, together giving a prognosis of equal to or less than a 6-month life expectancy.
Referring providers need to be specific with their diagnosis:
- Need to provide supporting labs, imagining, consultant notes and office notes
- Consider the need for labs or imagining prior to referral
- Talk to the patient and family – what are the patients' goals (drive the bus)
- Think longitudinally and latitudinally, over time and what is happening right now
- Call the Hospice physician if unsure before referring to either routine Hospice or for GIP care
Pain Management & Symptom Management
- See the Pharmacists letter/Prescribers letter August 2021 and July 2012
- These documents provide an opioid conversion algorithm, and have equianalgesic dosing, charts for pain management.
- There are multiple other conversation tables available, pick 1 and then always use the same one
Oral Equianalgesic Dosing
Morphine- 30 mg- Always convert dose back to morphine when changing narcotics or changing route of administration, when calculating your new narcotic dose.
Codeine- 200-3– mg
Tramadol- 200-300 mg
Hydrocodone- 30 mg
Oxycodone- 20 mg
Hydromorphone- 7.5 mg
Methadone- Use tables
Fentanyl Patches- 2-4X stronger than morphine (fentanyl 25 mcg patch equals morphine 50-100mg without needing to convert mcg to mg).
Codeine – Some children are fast metabolizers (overdose)
Some adults can’t metabolize (10%).
Tramadol – Poorly excreted in renal failure, toxic.
Multiple possible side effects:
- 10% at risk for dizziness.
- N/V, Constipation, somnolence, urinary retention, miosis, restlessness, seizures (higher risk if on tricyclic) and hypoglycemia.
- Risk of serotonin syndrome if on SSRI drugs.
I do not use these drugs.
Hydrocodone – generally available as a combination drug with acetaminophen which makes it dose limited and hard to titrate. Do not use in renal failure.
Oxycodone – combination drug with acetaminophen a stand-alone drug in pill form and liquid. Liquid can be very concentrated 40mg/ml. There is an ER (extended release) formulation, not used in hospice. Do not use in renal failure.
Hydromorphone – pill, liquid or injectable. Can be very concentrated for subcutaneous infusion at 10mg/ml. Subcu pump limited to 1ml/hour. Better drug in renal failure. There is also an extended release hydomorphone.
Methadone – pill, liquid or injectable. Only liquid narcotic that can be given 3x a day. Can be very concentrated for oral use, 50mg/ml. Excellent choice for opioid rotation, best drug for renal failure. Excellent for visceral pain and low dose excellent for neuropathic pain.
Fentanyl Transdermal Patches – good for chronic pain, not good for unstable or uncontrolled pain. Patches need 18+ hours to reach a study state, poorly absorbed in wasting patients, rapidly absorbed in febrile patients. Marijuana can ↑ dose by blocking cytochrome metabolizing system. Fentanyl patches follow the rules of all extended-release narcotics (see-later).
Morphine – pill, liquid, injectable and topical. 1st choice in Hospice pain management. There is a good oral concentrate @ 20mg/ml. It has the least interactions with other drugs. Easy to titrate. Cheap. Gold standard. Common to get red streak up arm with rapid IV administration, histamine release, not allergy.
Gabapentin – comes as a pill, titrate up to 3600mg/d for neuropathic pain. Titrate up over 1 month.
Lorazepam – pill, liquid or topical. Excellent for anxiety, agitation, and augmentation of narcotics.
Haloperidol – pill, liquid or injectable. Excellent for nausea, anxiety, agitation, delirium. Can give up to 5mg/hr until patient settles (delirium). Do not use on Parkinson’s Disease or Lewy Body Dementia.
Diphenhydramine – pill, liquid or injectable. Excellent to augment sedation and to treat or prevent dystonias. I use it when I am using high dose Haloperidol and use the injectable orally (less volume).
Miacalcin – nasal spray. Can be used for vertebral compression fractures (pathologic), and other bone pain. Use for 1 month. Consider bisphosphonates.
Dexamethasone- pill, liquid, or injectable. Good for appetite, sense of well-being, bone pain, hollow organ obstruction, brain metastasis, N/V and COPD.
Methylphenidate – pill. Can be used for incidental pain, repeated stabs of pain all over (multiple in a minute), refractory to narcotics. It can also increase appetite and sense of well-being in the elderly. 2.5 – 5mg before breakfast and lunch.
Ketamine – oral suspension, used at the HOC for uncontrolled pain, neuropathic pain, and agitation in actively dying patients. Can also be used on wounds before cleaning and dressing (as well as lidocaine gel).
Hypodermoclysis – subcutaneous – 1 liter a day with delirium or terminal agitation.
Other Medications:
Acetaminophen, NSAIDS, Oxybutynin (bladder spasm), Baclofen (hiccups), nystatin swish and swallow, nystatin powder, hydrocortisone cream 1%, Bacitracin (not Neosporin-rash), oxygen…
Pain Management
- Morphine does not mean death is imminent.
- Morphine does not kill hospice patients.
- Respiratory arrest does not occur with control of severe pain with morphine, even in “industrial” doses.
Do not use a 2nd class of short acting narcotics for breakthrough pain if the patients only pain medication is another class of short acting narcotics.
- Do not initiate extended-release narcotics until the patient has been on at least 40mg of immediate release morphine or its equivalent for at least 1 week. The FDA states that opioid tolerance only occurs after 1 week or more of short acting morphine 60mg or its equivalent dose.
- Try and avoid multiple classes and routes of narcotics
- Try to avoid narcotic/acetaminophen combinations.
- void codeine (Tylenol #3) and Tramadol
Pain & Symptom Management
Opioid Rotation:
- Rotate (see above) if escalation (significant escalation) does not control pain, or if pain seems to break through after a few days.
- Rotate if there appears to be opioid toxicity; myoclonus, irritability, acrodynia, or significant confusion without pain relief.
- Determine the morphine equianalgesic dose of the narcotic you are using and use the dose in calculating a new narcotic. Only start at 50% of the morphine equianalgesic dose with generous PRN’s. Use your equianalgesic table. Hydromorphone good choice, methadone also a good choice.
The European Society of Medical Oncology recommends a 3-step analgesic ladder.
- Mild Pain – Acetaminophen or NSAID’s.
- Moderate pain – weak opiates such as Tramadol or Codeine, or low dose Morphine can also be used (EAPC (European Association for Palliative Care).
- Moderate to Severe pain – Oral morphine if no help changes opiates or move to subcutaneous or IV opiates. Schedule.
- Fentanyl or Buprenorphine patches should only be used for those who cannot swallow.
Break through or rescue pain management:
- The Prescribers letter13 and the National Comprehensive Cancer Network5 recommend aggressive rescue for uncontrolled pain.
- Use 10-20% of the total hour dose of opioid as a rescue dose and repeat every 60 minutes with a 50-100% increase from the initial dose if needed. If using subcutaneous or IV, use 15-minute intervals.
- f no improvement after 3 cycles, consider changing PO to subcutaneous or IV. If already IV, change opioid or reassess. When pain is controlled, you can then incorporate the increased rescue dosing into the extended-release dosing. Do not schedule rescue or breakthrough meds.
Hospice Death (not Death with Dignity)
- Comfort/Passive Euthanasia:
- Always turn defibrillator off (not pacemaker).
- Withhold/withdraw life sustaining treatments.
- Increase medications to arrest pain (which may hasten death).
- Terminal sedation
All the above are legal.
Cachexia16 loss of lean body weight
Megestrol acetate – progesterone derivative – May increase appetite but not quality of life (diarrhea, rash, edema, thromboembolism, impotence).
Cannabinoids-Dronabinol or actual marijuana or oral or smoked marijuana products – No evidence-based data (Dranabinol approved by FDA or AIDs nausea).
Corticosteroids – Increase appetite, decreases fatigue, decreases bone pain/SOB, significant side effects over time(may increase fat but not muscle mass).
Cytokines/Neurohormones – Growth hormone agonists – no evidence-based data available at this time.
Nutritional Supplements – No evidence-based data, but “can’t hurt”.
- When you convert from one class of narcotic to another, consider giving ½ the equianalgesic dose initially with ample breakthrough (PRN) dosing. You can recalculate each day, adding up the PRN’s and adding 25-100% or that amount to your daily dosing.
- Do not change drip rates for at least 8 hours, preferably longer, increase the PRN’s.
- Augment – augment- augment. Lorazepam, Haloperidol, Prochlorperazine, Ondansetron, and Sertraline (or other anti-depressants).
- Give narcotics frequently (every 4 hours or more often) and in appropriate doses. Do not treat with only PRNs.
Delirium
Haloperidol and Lorazepam together are superior to Haloperidol alone in managing agitation and comfort in acute delirium in patients. Large frequent doses may be needed.
Constipation
- Have a plan for constipation starting on day one of pain management. This is the most important part of pain management.
- Stool softeners and stool laxative.
Closing Thoughts
- Consider all patients with life ending illness for hospice, or if they want life sustaining treatment with symptom management, to palliative care.
- Talk to your patients and their families about dying – use real words. AD, POLST.
- Refer early. Patients can have an informing visit without obligation to accept the hospice benefit and can have these visits more than once.
- Hospice patients can accept the hospice benefit, revoke, and again accept the benefit multiple times without penalty.
- Stop most medications.
- Use 1, or at the most, 2 classes or narcotics.
- Provide clear documentation and records with an appropriate/accurate hospice referral diagnosis.
- Upon referring a patient to hospice, the Hospice Physician and admitting RN can then work with you to qualify most all patients for the hospice benefit.
- Use Fentanyl patches less often and with great care, and never as the 1st narcotic.
- Upon discharge from the hospital to home the patient or family needs to have in hand;
- Morphine 20mg/ml, 15ml, 5mg-10mg Q4 PRN
- Lorazepam 2mg/ml, 15ml, or tablets, 0.5 mg #20, 0.5mg-1.0mg PO Q4 PRN
- Haloperidol 1.0 tablets #10, 1-2 mg every 6 hours as needed for nausea/agitation even if the patient has no pain.
- Upon discharge to custodial care, the patient needs scripts for the above medicines.
- GIP referral to a Hospice House or hospital- the patient needs to be in a symptom crisis that cannot be managed in another setting (or in current setting if in the hospital already).
- All Hospice appropriate patients need a referral from a provider, and then an informing to be admitted to home or GIP Hospice (Hospice House or hospital GIP).
- Talking with me may approve the hospice admission but a referral and informing still need to occur.
- Appropriate information needs to be provided to support either type of admission.
- Do not be afraid of good pain control. Hospice patients do not die from opiates.
- Co-manage your patient, if you choose, input and management discussions are encouraged.
- Hospice has a waiver with DHHS opiates rules but be aware of diversion and the need for universal precautions in some situations.
- Treat pain without anxiety or fear at the end of life.
Resources
Medscape, Palliative Cancer Care Guidelines. Updated: Feb 02, 2017. Author: Winston W. Tan, MD, FACP; Jessica M McMillan, DNP, ARNP, FNP-BC
Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of Palliative Care into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice guideline update. J clin oncol. 2017 Jan. 35 (1) : 96-112
NCCN Clinical Practice Guidelines in Oncology Palliative Care Version 1.2016 National Comprehensive Cancer Network. Available at http:/www.nccn.org/professionals/physician_gls/pdf/palliative.pdf
NCCN Clinical Practice Guidelines in Oncology Adult Cancer Pain. Version 2.2016 National Comprehensive Cancer Network
National Hospice and Palliative Care Organization Facts and Figure. Hospice Care in America. 2016 Edition. September 2017. P 1-9
PL Detail Document, Opioid Conversation algorithm. Pharmacists letter/prescribers letter. August 2012.
PL Detail Document, Equianalgesic Dosing of Opioids for Pain Management. Pharmacists Letter/Prescribers letter. July 2015.
David Hui, MSC, Susan Frisbee-Hume, MS, Annie Wilson, MSN, et al. Managing acute Delirium in the last days of life. JAMA 2017; 318 (11): 1047-1056
Stephen R. Connor PhD, Bruce Pyenson, FSA, MAAA, Kateryn Fitch, RN, MA, Med, Carole Spence, RN, MS, and Kosuke Iwasaki, FIAJ, MAAA. Comparing Hospice and Non-Hospice patient survival among patients who die within a 3 year window. Journal of Pain and Symptom management. Vol 33 no. 3 March 2017: 238-246
Bruggerman, et al. J Oncol Pract. 2016; 12 (11): 1047-1056
TESTIMONIALS
What People Say About Us
“The House of comfort is a wonderful facility for end-of-life care. My Dad went for a week of respite care, and I can't thank the staff enough for all they do. It really is a "House of Comfort." I felt very much at home when visiting Dad. The atmosphere is of a quiet nature. There are various sitting areas, a fireplace, and a kitchen area. The staff are friendly and there for you and your loved ones anytime, day or night. I love you, Pop. From the bottom of my heart, I say "thank you" to the entire staff at the House of Comfort.”
Becky Hare
“When my father, Danny Albert, was at the House of Comfort, I felt so incredibly thankful that my family and I could be there with him in such a beautiful and supportive environment, during that part of his journey. It’s a bizarre feeling to be suffering and grieving while in a place of peace. The House of Comfort is (surprisingly) exactly that, a place of peace that lifts the weight of tragedy off your shoulders enough so you can breathe and be present, knowing your loved one is being cared for.”
Kelsey Anderson
Support the Aroostook House of Comfort
Your gift helps provide inpatient hospice care to the people of Aroostook County.




